The COVID-19 crisis has revealed the harmful consequences of leaders making critical decisions based on insufficient data, which end up hurting the most vulnerable communities.
With many people impatient to get back to work and businesses eager to re-open, experts agree that widespread and ongoing diagnostic and antibody testing for COVID-19 are essential for any plan to return to normal.
However, there are major hurdles to overcome, from having accurate data on infections and better demographics data on those most affected, to a better understanding of how the virus spreads and the variation in severity of cases.
Unfortunately, as some states move to re-open, they are making these decisions in the dark and putting people's lives at risk.
The U.S. had a slow start rolling out testing, hindering data on COVID-19 infections early on. The first batch of tests made in mid-February by the Centers for Disease Control and Prevention (CDC) were unusable because the CDC didn't follow its own protocol and contaminated the tests. Now with ramped up testing, private labs are facing major backlogs because they didn't want to turn away business, even though they lacked the capacity to run all the tests they accepted.
There is concern that because most states are not providing information on pending tests, the extent of outbreaks is being under-reported. Meanwhile, academic labs are operating below capacity. Further, the tests require validation, as some have poor accuracy and could dangerously lead to false negatives.
While this train wreck is on public display, it's a familiar landscape to those of us who work in the field of chemical regulation.
What we don’t know could kill us
The U.S. Environmental Protection Agency (EPA) routinely makes decisions in the dark. Its chemical regulation arm approves chemicals, often toxic to humans, to market without adequate data on safety.
The EPA often assumes lack of data is equivalent to safe. Only if there is a massive tragedy linked to a chemical, such as the effects of lead on brain damage in children, do regulators consider health.
Just like doctors, businesses, and government leaders today are calling for more COVID-19 testing before opening up the country, environmental health scientists routinely call for more chemical safety testing before chemicals are put on the market.
Currently, the EPA is conducting risk evaluations for a number of chemicals that have been in use for decades to decide if they should be withdrawn. Five of the chemicals in question are linked to breast cancer.
At the same time, EPA is considering approval of six new PFAS chemicals. PFAS are a class of "non-stick" chemicals widely used in consumer products that have been linked with cancer, have contaminated our drinking water, and are found in the blood of virtually every American.
Last year the EPA approved three new PFAS, despite incomplete test results, failed test protocols, and enormous data gaps on the health effects, as we detailed in our comment to EPA.
As with COVID-19, what we don't know could literally kill us.
Medical and environmental racism
What we do know is that communities of color are being hit harder by COVID-19. Medical racism, poor access to good health care, and chronic exposures among essential service workers are important contributing factors.
However, a lack of systematic data collection and reporting of racial data is preventing these communities from receiving the necessary level of care and resources.
These disparities are common in environmental justice work, where communities of color experience higher levels of air pollution.
Now there is evidence that air pollution increases vulnerability to COVID-19.
A renewed focus on prevention
Inadequate chemical safety regulations, along with a stream of environmental rollbacks under this administration, will have lasting impacts long after this pandemic is over.
To protect ourselves from future pandemics, safeguarding our environment, reducing hazardous exposures, and building a stronger evidence-based public health system are essential.
But, in order to do that, we have to correct 50 years of dwindling investments in public health.
In 2019, just 4 percent of the National Institutes of Health budget went toward prevention. And yet, as we've seen with COVID-19, prevention is powerful; states that issued stay at home orders earlier rather than later undoubtedly saved countless more lives.
It is now clearer than ever that as a society, we need a stronger public health infrastructure, one that focuses on prevention and relies on sound science to make decisions.
Kathryn Rodgers is a staff scientist at Silent Spring Institute, based in Newton, Massachusetts.
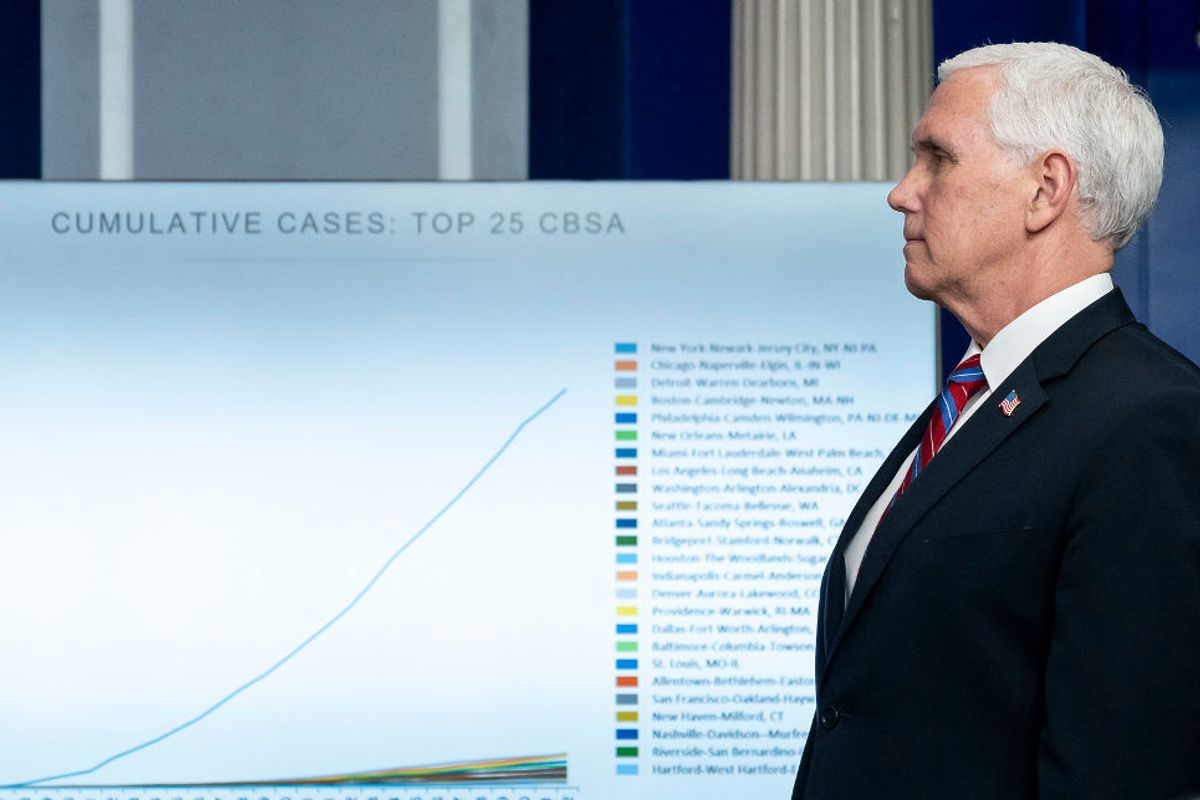
Banner photo: Vice President Mike Pence listens as White House Coronavirus Task Force Response Coordinator Deborah Birx delivers her remarks during the coronavirus update briefing Monday, April 13, 2020. (Credit: The White House)